
Expert Pain Relief, Close to You
As a busy, tech-forward clinic we combine evidence-based care, professional training, and clinical research to deliver comprehensive pain management. Specialising in non-pharmacological pain relief, we offer advanced therapies including physiotherapy, acupuncture, chiropractic, therapeutic massage, herbal medicine, and integrative treatments — providing expert care for the treatment and relief of various pain conditions.
- 7-Day Clinic (Monday To Sunday) – No Need To Wait.
- ACC & Major Insurances
- No ACC? No Problem. Affordable Price, Afterpay, MSD Available.
- New Patients Free Trail.
- Multilingual Support: English, 中文, हिंदी
Jada is an excellent massage therapist who was able to identify my pain points and treat them effectively.
I highly recommend this clinic — they don’t just focus on pain relief, but also provide genuine care and emotional support throughout the session.
The team were incredibly lovely and welcoming. Jada was excellent!!!
---
Life-changing experience with Dr. Alan!
I came to Dr. Alan suffering from severe menopausal symptoms — constant hot flashes, extreme fatigue, and recently discovered I had very high blood pressure and cholesterol. I honestly didn’t know what to expect, but the results were immediate and incredible.
As soon as Dr. Alan began acupuncture, I felt an instant cooling sensation from my head — something I hadn’t experienced in months. He also pressed on points around my body where I screamed in pain, and each time, when he inserted the needles, the pain disappeared within seconds. It felt like a huge pressure was lifted off my whole body.
Dr. Alan is not only highly skilled but also extremely sincere and caring. He took the time to explain in detail the underlying causes of my issues, describing how the blockages were affecting my body. His knowledge and compassion made me feel completely at ease.
I walked out of the clinic feeling lighter, calmer, and truly renewed — it was like my entire body finally started to breathe again. I can’t thank Dr. Alan enough for his amazing work. Highly recommend him to anyone struggling with pain, fatigue, or hormonal symptoms. He’s a true healer
I especially want to mention Alan, who is truly outstanding. He takes the time to listen carefully, explains everything clearly, and tailors each session to your needs. His skills in acupuncture and massage are amazing — after just a few treatments with him, my long-term neck and back pain improved dramatically. Alan is not only highly knowledgeable but also very caring and attentive, which makes every session both effective and comfortable.
If you are looking for a place that provides genuine results with a professional and supportive approach, I couldn’t recommend this clinic more. A great environment, a very professional team, and special thanks to Alan for his excellent care.
Heal Naturally starting from free trial
Explore our integrative, drug‑free treatments—physiotherapy, acupuncture, and massage—designed to relieve your pain, restore mobility, and enhance your quality of life.
We offer free trial on all our services and membership is starting from just $100 for your huge savings.


Rediscover Comfort with our affordable Prices
Learn how our personalized care plans address the root causes of pain, combining evidence‑based techniques to deliver lasting relief and empower you to live pain‑free – all at very affordable prices.
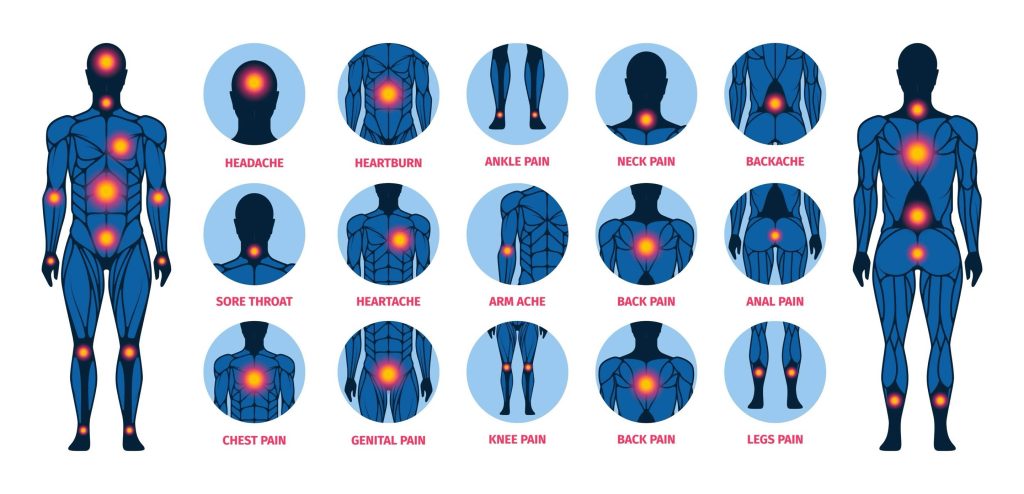
What we are treating?
We treat most of the body pain for you in the natural way.
Head Pain

Headaches occur when blood vessels, muscles, nerves, or tissues around the brain and cervical spine are irritated, or from chemical imbalances. Main types include tension headaches from stress or neck strain, migraines triggered by hormones, foods, or poor sleep with throbbing pain and sensitivity, and cervicogenic headaches caused by neck dysfunction. Triggers include poor posture, screen use, eyestrain, dehydration, and jaw clenching.
Auckland Pain Management Clinic uses acupuncture, manual therapy, cupping, physiotherapy, and neuromodulation for relief. At home, patients should maintain ergonomics, stretch, apply warm compresses, stay hydrated, and practice mindfulness.
Neck Pain

Neck pain occurs when cervical muscles, joints, nerves, or discs become irritated or strained. Common causes include muscle overuse, whiplash, herniated discs, arthritis, or poor posture from prolonged desk/device use. In Traditional Chinese Medicine, it may stem from Qi stagnation, wind-cold invasion, or meridian imbalance.
Symptoms range from stiffness, reduced motion, and spasms to radiating pain, headaches, numbness, or tingling in the arms.
Effective care combines physiotherapy for alignment and strength, acupuncture for circulation, manual therapy for tension release, and cupping or TENS for nerve pain.
At home, patients should maintain ergonomic posture, stretch daily, apply warm compresses, avoid poor sleeping positions, and use supportive aids like heat wraps or neck massagers.
Wrist & Hand Pain

ChatGPT said:
Wrist and hand pain often results from repetitive strain, tendon inflammation, nerve compression, or joint degeneration. Conditions include carpal tunnel, De Quervain’s tenosynovitis, and arthritis. At Auckland Pain Management Clinic, treatment begins with detailed assessment, followed by physiotherapy (strengthening, stretching, ergonomic advice), acupuncture to enhance circulation and nerve repair, and manual therapies to mobilize joints and release tendons. Scraping therapy along the wrist and forearm further eases tightness.
At home, patients should use ergonomic devices, take breaks, apply warm or cold packs, perform gentle stretches, and wear night braces for carpal tunnel relief. Supportive patches may also help.
Should & Arm Pain

ChatGPT said:
Shoulder and arm pain often arises from rotator cuff strain or tears, frozen shoulder, bursitis, cervical nerve compression, poor posture, or repetitive lifting. Symptoms include aching or sharp pain, stiffness, weakness, numbness, tingling, and night discomfort.
At Auckland Pain Management Clinic, care starts with thorough assessment of joint, muscle, and nerve function. Physiotherapy restores mobility and strength through guided exercises and posture correction. Acupuncture reduces inflammation, while manual therapy, cupping, and Gua Sha release tight tissues and improve circulation. Electroacupuncture or TENS provides targeted relief for nerve-related pain.
At home, patients should avoid heavy lifting, use ice or heat, practice pendulum and wall-crawl exercises, and maintain good posture. Braces, compresses, patches, and massagers further support recovery.
Back & Hip Pain

Back and hip pain often result from lumbar strains, disc issues, sacroiliac dysfunction, sciatica, arthritis, or poor posture—sometimes explained in TCM as cold-damp invasion. Symptoms may include dull or sharp pain, stiffness, spasms, reduced mobility, and radiating leg numbness.
At Auckland Pain Management Clinic, treatment begins with assessment of spinal alignment, core strength, and gait. Physiotherapy restores balance through strengthening and posture correction, while acupuncture eases inflammation. Manual therapies, cupping, and Gua Sha improve mobility, and electroacupuncture or TENS target stubborn nerve pain.
At home, patients should alternate heat therapy with movement breaks, stretch daily, and maintain proper sleep posture. Lumbar supports, foam rollers, braces, and herbal patches further aid recovery and long-term prevention.
Knee & Leg Pain

Knee and leg pain often stems from osteoarthritis, ligament or meniscus injuries, runner’s knee, IT-band tightness, muscle imbalance, poor biomechanics, or—per TCM—meridian blockages. Symptoms include aching or sharp joint pain, swelling, stiffness, clicking, and instability.
At Auckland Pain Management Clinic, care begins with assessment of joint alignment and movement. Physiotherapy strengthens supporting muscles, retrains gait, and restores balance. Acupuncture reduces inflammation, while manual therapy, cupping, and Gua Sha release tight tissues. Electroacupuncture or TENS offers relief for persistent or radiating pain.
At home, patients should alternate ice and heat, elevate legs, perform gentle mobility exercises, and favor low-impact activities like cycling or swimming. Supportive footwear, braces, foam rollers, and massagers enhance recovery and prevent recurrence.
Ankle & Foot Pain

ChatGPT said:
Ankle and foot pain may arise from sprains, plantar fasciitis, Achilles tendinitis, flat feet, arthritis, or nerve compression. In TCM, it can reflect Qi stagnation, cold-damp invasion, or kidney deficiency. Symptoms include swelling, bruising, stiffness, instability, heel pain, or tingling sensations, often aggravated by weight-bearing or poor footwear.
At Auckland Pain Management Clinic, treatment starts with biomechanical assessment. Acupuncture reduces inflammation and aids healing, while manual therapies—joint mobilization, fascia release, and calf work—restore mobility. Gua Sha and physiotherapy strengthen stabilizers and retrain balance to prevent recurrence.
At home, patients should rest and elevate the limb, use cold packs for sprains or warm soaks for stiffness, wear supportive shoes, and practice daily stretches. Braces, rollers, and herbal soaks further enhance recovery.
Joint Pain

Joint pain may arise from osteoarthritis, rheumatoid arthritis, gout, repetitive strain, or trauma, presenting as pain, stiffness, swelling, reduced mobility, and sometimes deformity. In TCM, it is seen as “Bi Syndrome,” where wind, cold, damp, or heat obstruct Qi and blood.
At Auckland Pain Management Clinic, treatment starts with joint and alignment assessment. Physiotherapy improves biomechanics through strengthening and retraining. Acupuncture reduces inflammation and pain, while manual therapy, cupping, and Gua Sha restore circulation and ease stiffness. Heat or infrared therapy supports chronic cases.
At home, patients should apply warm compresses, practice low-impact exercise like swimming or Tai Chi, protect joints from cold/damp, and use braces or cushions when needed. Maintaining healthy weight, using warming oils, and gentle massage further reduce stress and aid recovery.
Adomen Pain

ChatGPT said:
Abdominal pain may arise from digestive issues (IBS, indigestion, constipation, food intolerances), muscular strain, reproductive concerns, or nerve irritation. In TCM, causes include cold invasion, food stagnation, sluggish liver Qi, blood stasis, or spleen/kidney deficiencies. Symptoms range from cramping, bloating, and sharp pain to nausea, irregular bowels, or menstrual cramps.
At Auckland Pain Management Clinic, treatment begins with a detailed assessment. Acupuncture harmonizes organ function and relieves spasms, while gentle abdominal massage, fascial release, and breathing exercises ease tension. Moxibustion warms meridians, and cupping supports circulation and organ regulation.
Patients also receive lifestyle guidance on diet, stress management, and posture to improve digestion and prevent recurrence—empowering them to restore balance and daily comfort.
Period Pain

Period pain often results from uterine contractions and prostaglandin-driven inflammation, and may be worsened by endometriosis, fibroids, or—in TCM—cold retention and liver/kidney deficiencies. Symptoms include lower abdominal cramping radiating to the back or thighs, nausea, fatigue, bloating, and irritability.
At Auckland Pain Management Clinic, care begins with menstrual history and lifestyle assessment. Acupuncture regulates Qi and blood flow, while moxibustion warms the uterus and relieves tension. Gentle abdominal massage and sacral release further ease discomfort.
At home, patients can use warm compresses, drink ginger or cinnamon tea, stretch gently, and avoid cold foods or drinks. Heat wraps and herbal patches provide added relief, helping restore comfort and balance during cycles.
Shingles Pain

Shingles pain arises from reactivation of the varicella-zoster virus, often leaving lingering postherpetic neuralgia with burning, stabbing, or electric-shock sensations. Risk factors include low immunity, delayed treatment, and—in TCM—patterns like liver fire, damp-heat, or Qi stagnation.
At Auckland Pain Management Clinic, treatment starts with careful assessment. Acupuncture reduces nerve hypersensitivity and restores meridian flow, while low-level laser and gentle cupping aid nerve repair. Herbal formulas clear damp-heat, nourish Yin, and support immunity, and manual therapy improves circulation and eases tension.
At home, patients should keep the area clean, avoid friction, wear loose clothing, and apply warm compresses. Stress management, cooling diets, and supportive tools like herbal patches, balms, or moxa rolls further relieve pain and promote healing.
Body Pain
ChatGPT said:
Generalized body pain may stem from muscle fatigue, chronic inflammation, poor sleep, stress, or post-viral fatigue. Conditions like fibromyalgia and chronic fatigue syndrome are common causes, while in TCM, patterns include Qi and blood deficiency, damp-cold invasion, or meridian stagnation. Symptoms often involve widespread aching, heaviness, stiffness (especially in the morning), and low energy.
At Auckland Pain Management Clinic, treatment combines physiotherapy for posture correction, stretching, and electrotherapy with acupuncture to boost circulation and calm the nervous system. Manual therapies release tension, while herbs and moxibustion strengthen Qi, dispel dampness, and improve immunity.
At home, patients are advised to maintain good sleep, stay warm, practice gentle movement like yoga or Tai Chi, eat warm nourishing foods, and use infrared heating pads. Body massagers, herbal teas, and ergonomic bedding further aid comfort and recovery.
Chronic Pain

ChatGPT said:
Chronic pain is defined as discomfort persisting beyond three months, often linked to poorly healed injuries, inflammation, or neuropathic conditions like sciatica or postherpetic neuralgia. In TCM, it reflects Qi and blood stagnation, organ deficiencies, or cold-damp retention. Symptoms include ongoing dull, sharp, or burning pain, fatigue, sleep disturbance, reduced function, and emotional stress that worsens perception.
At Auckland Pain Management Clinic, treatment combines physiotherapy for strength and mobility, acupuncture to regulate the nervous system, herbal medicine to restore balance, and manual therapy for tissue release. Moxibustion addresses cold-type pain, while mind-body support and diet guidance enhance outcomes.
At home, patients are encouraged to maintain good sleep, use relaxation practices, apply heat or cold packs, stay active, and use ergonomic supports, massage devices, or herbal balms. These strategies promote recovery and long-term comfort.
Nerve Pain

Nerve pain, or neuropathic pain, arises from nerve damage or dysfunction, often described as burning, stabbing, tingling, or electric-shock sensations. It may result from conditions such as sciatica, shingles, diabetes, trauma, or nerve compression, and is often persistent and disruptive to sleep, mood, and daily function.
At Auckland Pain Management Clinic, we take an integrative approach combining physiotherapy to improve posture and relieve pressure, acupuncture to calm nerve hypersensitivity and restore flow, and manual therapies to release tight tissues. Electroacupuncture, TENS, and herbal support further ease discomfort, helping patients reduce pain, regain confidence, and restore quality of life.
Pediatric Pain

Pediatric pain can arise from injuries, post-surgical recovery, growing pains, headaches, or chronic conditions, and may present as irritability, sleep disturbances, or reduced activity since children often struggle to express discomfort clearly. Effective management requires gentle, age-appropriate care that addresses both physical and emotional needs.
At Auckland Pain Management Clinic, we provide a supportive environment for children and families. Treatments may include physiotherapy for mobility and posture, acupuncture with child-friendly techniques to reduce pain and calm the nervous system, and gentle manual therapies to ease tension. We also guide parents on home strategies to promote comfort and resilience.
Pediatric Pain
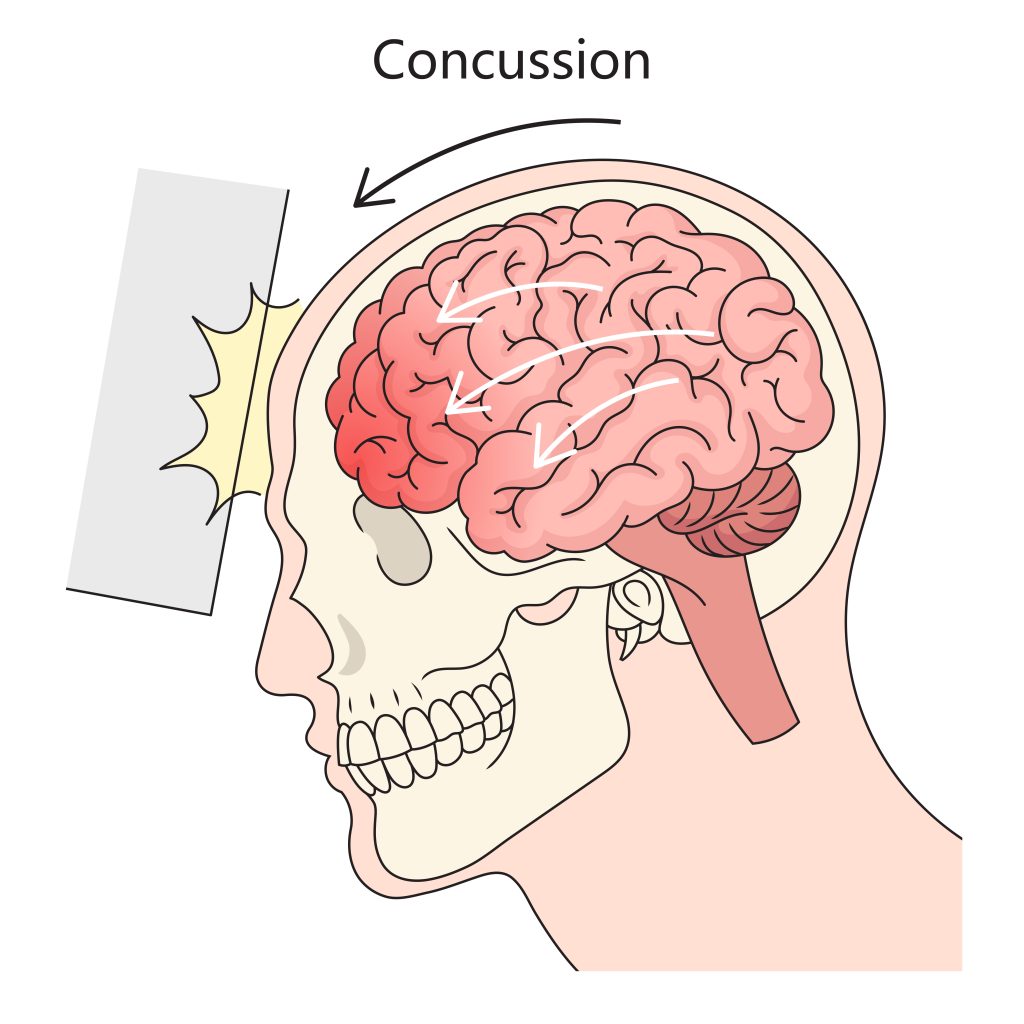
A concussion is a mild traumatic brain injury caused by impact, sudden movement, or whiplash, leading to temporary disruption of brain function. Symptoms may include headache, dizziness, nausea, confusion, blurred vision, memory issues, or sensitivity to light and noise. Though often short-term, repeated concussions or poor recovery can cause lasting effects.
At Auckland Pain Management Clinic, we support recovery with a holistic approach—physiotherapy for balance and neck stability, acupuncture to reduce headaches and calm the nervous system, and gentle manual therapy to ease muscle tension. Lifestyle guidance on rest, sleep, and gradual activity helps restore clarity and resilience.
Pre&post-op rehabilitation

Pre- and post-operative rehabilitation focuses on preparing the body for surgery and supporting recovery afterward. Before surgery, targeted exercises, posture training, and breathing techniques improve strength, circulation, and resilience. After surgery, rehab reduces pain, restores mobility, prevents complications, and accelerates return to normal function.
At Auckland Pain Management Clinic, we provide individualized care combining physiotherapy for strength and mobility, acupuncture to reduce inflammation and support healing, and manual therapies to ease tension and scar tightness. We also guide patients with safe home exercises, posture correction, and lifestyle strategies, ensuring smoother recovery and better long-term surgical outcomes.
What We’re Offering
We offer variety of services to suit your needs
Fast Pain Relief By Stimulating Specific Points To Reduce Inflammation And Block Pain Signals.
Restores movement and reduces pain through targeted exercise, manual therapy, and education.
Relieves muscle tension, improves circulation, and eases chronic and acute pain.
Promotes blood flow and releases muscle tightness for effective pain relief.
Aligns the spine and joints to reduce nerve irritation and musculoskeletal pain.
Uses natural plant-based remedies to support healing and relieve pain without drugs.
01.
Post-Surgery Recovery
Lorem ipsum dolor sit amet elit. Curabitur posue ipsum eu malesuada iaculis.

02.
Chronic Pain Relief
Lorem ipsum dolor sit amet elit. Curabitur posue ipsum eu malesuada iaculis.


03.
Mobility Restoration
Lorem ipsum dolor sit amet elit. Curabitur posue ipsum eu malesuada iaculis.

04.
Muscle Tension
Lorem ipsum dolor sit amet elit. Curabitur posue ipsum eu malesuada iaculis.
Browse Our Online Shop
We Sell top quality Physio Products
Massager
Herbal Oil
Protective Equipment
Others
Relief of your pain from $0 with our Free-trial services
Auckland Pain Management Clinic offers Free trial on our services to new customers. we’ll grant you:
- Physiotherapy Free Trial
- Acupuncture Free Trial
- Relaxing Massage Free Trial
Once you are happy with our services and/or therapies, you are welcomed to order the VIP membership for great savings or pay per visit.


How it works
Interested? let’s get started here
1. Start for free
Free First trial
- Massage 10
- Physio 30 min.
- Acupuncture 30 min.
- Free Physio for ACC Claims (no referral required)
2. Stay for relief
Professional Pain Relief
- Experienced & Registered Practitioners
- Rapid, effective, and lasting pain relief.
- Advanced Drug-Free Integrative Therapies
3. Save with our price
Affordable member pricing
- $50-$60 for 1 hour Massage.
- No Surchargefor ACC Session
- $50for Private Session (Physio, Acupuncture).
- FreePhysio for ACC Claims (no referral required)
Real Success. Real Change
*Testimonials are actual comments from our Google Reviews
Our Team
Our professionals are here to meet you requirements and relief your pain. Meet them today!
Testimonials
See what our customer says about Pain Management Clinic
Join Our Team?
We are actively looking for good people to join our team. To apply, please send your resume to pmc@painclinic.co.nz
Current Open Positions:
If you know a friend or colleague who’d be perfect, refer them! When they apply and mention your name, you’ll receive a $1,000 referral bonus. Just send us a quick email to let us know you’ve referred someone.

























